Nose job

If you were to ask certain celebrities, including Jennifer Aniston and Cameron Diaz, they’d likely say their nose jobs were medically necessary. The truth is a bit more complicated. Rhinoplasty, sometimes referred to as a “nose job,” can be performed to correct impaired breathing caused by structural defects of the nose (such as a deviated septum), but it also—and often—includes aesthetic tweaks to enhance facial harmony and the proportions of the nose. Insurance covers the portion of the surgery that can be shown to be medically necessary. That’s good news when you consider that the average surgeon charges $5,046 for a rhinoplasty. What’s not so good news is that Dr. Johnson says that typically, “once we’ve finished the structural work, we mark the time on the operative record,” and after that, it’s on the patient’s tab. There may be savings by combining the structural with the aesthetic, as compared with doing two separate surgeries, however. For example, by combining the surgeries, the patient may be able to do only one set of pre-operative evaluations (such as blood work).
Ears

No one wants to earn the nickname “Dumbo.” But the sad truth is that your ears continue grow throughout your lifetime. Ear surgery, also known as otoplasty, can improve the shape, position, or proportion of the ear. It can also correct a defect in the ear structure that is present at birth but became apparent only later or an ear misshapen by accident or injury. According to the ASPS, correction of even minor deformities can have profound benefits for appearance and self-esteem. Both adults and children can benefit from otoplasty, but if you make it to adulthood without it, then any changes you might want to make “will probably be on your dime,” Dr. Johnson says. Otoplasty in adults is covered by insurance, however, when it interferes with hearing. When it isn’t covered, the average cost is $3,154. Find out what your ear wax says about your health.
Eye job

Aging, sun exposure, and genetics can all contribute to wrinkles, puffiness, and sagging of the skin around the eyes, which can cause a woman to look tired or older than she is. The surgical remedy is blepharoplasty, commonly known as an eyelid lift. Blepharoplasty can be done on the upper lids, the lower lids, or both. Incisions are made in the skin crease of the upper lids and/or right below the lower eyelashes, and excess fat and skin are removed, giving the eyes a smoother and firmer appearance. But does insurance cover plastic surgery for the eyelids, which can cost an average of $3,022? Dr. Johnson says it actually will in two situations. The first is when extra skin weighs down the eyelid, obstructing the patient’s vision. The second is when the muscles of the upper lid become stretched out over time, leaving the patient with a sleep-eyed look that also impairs vision. Patients seeking coverage may be required to present documentation from an eye doctor. Here’s how dermatologists and plastic surgeons look younger without an eyelid lift.
Content continues below ad
“Beauty” marks

You’ve heard it called a beauty mark, but you don’t think it’s so beautiful. If you decide to have that mole removed, will insurance cover it? According to Dr. Johnson, “even if the mole turns out to be benign, insurance will usually cover its removal if it strikes a doctor as suspicious.” Suspicious moles include moles that have grown or shrunk or otherwise changed, moles with a diameter larger than a pencil eraser and moles that bleed or itch. If it does turn out to be cancerous, Dr. Johnson adds, “your insurance plan should also cover surgery to reconstruct your appearance.” As with most of these surgeries, pre-certification is generally required for reimbursement or coverage, so be sure to consult with your insurance company in advance of any surgery.
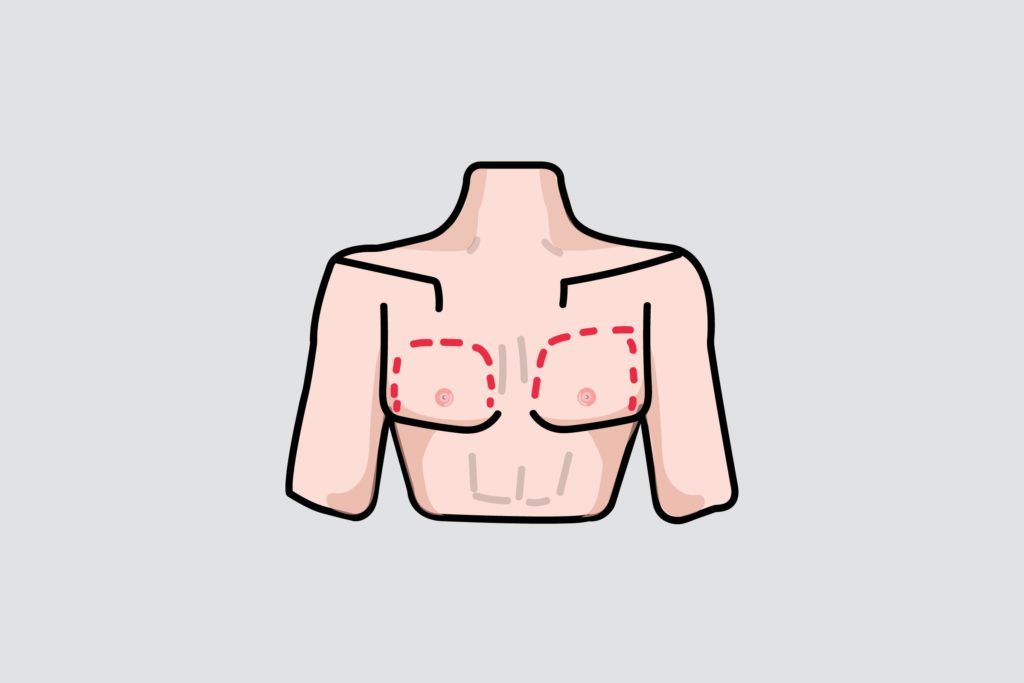
Boob jobs

Breast augmentation costs Americans more than a billion dollars last year (with each surgery costing an average of $3,719 for the physician’s fee alone, not including anesthesia, operating room facilities, and related expenses). So if you’re asking, “Does insurance cover plastic surgery?” then there’s a pretty good chance you’ve got breast augmentation on your mind. As you may suspect, your health insurance won’t pay for you to get yourself a bigger set just because you want them. However, there are circumstances when your insurance will pay. Plastic surgeon Deborah J. Johnson, MD, President of the American Society of Plastic Surgeons (ASPS), explains that when you talk about plastic surgery covered by insurance, the question always comes down to what is “cosmetic” versus “reconstructive.” “It’s cosmetic if it’s simply the altering of the normal to make it look better but still normal. Aging is normal, so if someone comes in for work on their breasts due to the normal aging process, we consider that cosmetic,” Dr. Johnson explains. “If it’s addressing functional disabilities and deformities, it’s reconstructive.” But the notion of what is “normal” and what is a “deformity” is constantly evolving, as Johnson points out.
Since 1998, insurance companies have been required by law to cover not only breast reconstruction following mastectomy but also reconstruction of the other breast to make breasts look symmetrical and balanced after mastectomy and any physical complications at all stages of mastectomy. This includes revising previous reconstructions, points out Maria LoTempio, MD, a New York-based plastic surgeon specializing in reconstructive and cosmetic surgery exclusively for women. That means that following an initial reconstruction, a woman can opt for a different reconstructive approach for the purpose of enhancing the aesthetic result. Dr. LoTempio notes that the likelihood of insurance covers diminishes as time passes following the initial reconstruction, although in one case, a patient received full coverage for significant revision nearly eight years following her initial surgery. Dr. Johnson suggests that patients read their plans carefully and work closely with customer service representatives at the insurance company to determine whether the desired surgery will be covered. A review of a paper prepared by the ASPS regarding a form of revision known as fat grafting (which transfers to the breast fat that’s been removed from other parts of the body via liposuction) indicates that insurance companies can vary widely in their coverage.
Apart from breast reconstruction, Dr. Johnson points out that women who have already undergone a “boob job” may be able to have the removal of their implants paid for by insurance if the implants are found by a doctor to be faulty. Although insurance won’t cover the replacement, most implants now come with a lifetime warranty. As such, the implant manufacturer will pay for the replacement, and some manufacturers go so far as to cover the operating room expense for 10 years following the initial implant surgery. Here’s everything you always wanted to know about breast implants.
Breast reduction

On the flipside is breast reduction surgery, the average cost of which is $5,631. During breast reduction, the surgeon removes fatty tissue, glandular tissue, and excess skin. Women may choose breast reduction to address both physical and emotional discomfort. Although insurance companies tend to use cup size as a guideline (often denying coverage if you’re not a “DD or larger,” notes Dr. Johnson), the ASPS recommends to insurance companies that the determination should focus not on how large the woman’s breasts are, but on the severity of a woman’s symptoms. For example, the weight of very large breasts can cause neck, shoulder, and back pain, leading to pain and discomfort during day-to-day activities. A woman may also experience rashes and yeast infections where her breasts fold over her torso. All of this may contribute to severe emotional pain as well.
“If her nipples are pointing to the floor, it’s obviously a problem,” says Dr. Johnson, “but it depends on the subjective thought process of the reviewer.” Dr. Johnson recommends documenting the symptoms and their duration (some insurance companies won’t consider paying for breast reduction until the symptoms have gone on for at least a year). She also recommends documenting all non-surgical measures taken by the woman that have failed (such as diet, exercise, supportive bras, chiropractic, and massage). It’s also a good idea to document the woman’s willingness to endure scarring in the interest of relieving her symptoms, Dr. Johnson adds, because this shows that her desire for the surgery isn’t frivolous.
Content continues below ad
Male breast reduction
The American Board of Cosmetic Surgery estimates that up to 50 percent of men in the United States will experience enlarged breasts during their lifetime. As with oversized breasts in women, enlarged breasts in men can present serious challenges, including pain, rashes, infections, and related emotional issues. For some men, the answer is gynecomastia surgery, which removes excess fat and glandular tissue for a flatter, firmer, and more masculine chest contour. Whether insurance will pay for the surgery, for which the ASPS says that surgeons charge an average of $3,525, depends first and foremost on the age of the patient.
In teenage boys, enlarged breasts are often the direct result of hormonal changes. Ninety percent of the time, the condition resolves on its own within three years. However, at a time when adolescents are already struggling with issues relating to sexual identity and self-image, the psychological distress associated with gynecomastia can be significant and debilitating. According to Dr. Johnson, insurance companies are more willing to pay for the surgery in teens and young adults than they are for older adults. There’s a common belief, she notes, that “if this guy made it through his teens and early twenties without the surgery, he’s fine.” In addition, enlarged breasts in adults are more easily linked to excessive body fat and to the normal aging process. Therefore, insurance companies tend to require proof that the adult patient has attempted to decrease his breast size through diet and exercise and often won’t consider covering surgery unless the enlargement is at least moderate to severe.
In some cases, gynecomastia presents along with male breast cancer. The presence of a suspected malignancy is another factor insurance companies consider when deciding whether to cover this surgery.
Panniculectomy

Major weight loss is a super-healthy step for those suffering from obesity. What isn’t super-healthy is the excess skin that remains. Excess skin can be heavy enough to cause physical pain. It can affect mobility, limit physical activity, and affect personal hygiene. Skin folds can become tender and become breeding grounds for yeast infections. Panniculectomy is a surgical procedure to remove the excess skin remaining after significant weight loss. When performed to correct or relieve physical symptoms, it is considered reconstructive and therefore subject to coverage by insurance. However, the law is still evolving in this area, according to Dr. Johnson. “There was a time a few years back when insurers covered panniculectomy. Then they decided it was a problem of one’s own making and began to deny coverage,” she recalls. “Then the American Medical Association classified obesity as a disease, and states began requiring insurance companies to once again cover the surgery.” If you’ve never heard of a panniculectomy, chances are that these unusual cosmetic surgeries will be news to you as well.
Tummy tuck

Whereas a panniculectomy removes only excess skin, a tummy tuck (also known as abdominoplasty) involves the removal of excess skin and fat from the abdomen and a tightening of underlying abdominal muscles. You might feel you need a tummy tuck after pregnancy, especially if your expanding belly causes your abdominal muscles to separate vertically (this is known as diastisis). However, insurance doesn’t cover diastisis repair, which is viewed by the medical profession as strictly appearance-enhancing, and that’s unfortunate considering that the average surgeon charges $5,798 for a tummy tuck. A tummy tuck will be covered by insurance, however, when it is done as part of a breast reconstruction. For example, in what is known as a DIEP Flap procedure, Dr. LoTempio uses skin and fatty tissue from the abdomen to replace the skin and tissue removed from the breast during mastectomy, resulting in a soft, natural, reconstructed breast. In SIEA Flap surgery, the blood vessels in the lower abdomen, just beneath the skin, are used. In either case, the contour of the abdomen can be smoothed and improved the way it is as a result of a cosmetic tummy tuck. Here are 23 ways to flatten your belly without surgery.
Content continues below ad
Butt lifts

The average surgeon charges $4,356 for buttocks augmentation, so wouldn’t it be nice if insurance would cover that Brazilian butt lift? It would, but that’s not happening. However, if you must undergo a mastectomy for medical reasons, there are surgeons who are able to create new breasts out of skin, fat, and blood vessels removed from the gluteal area. This surgery results in a newly contoured and lifted backside and is now routinely covered by insurance, although Dr. LoTempio can recall a time less than a decade ago when the road to obtaining coverage sometimes involved a lengthy and nerve-wracking appeals process. Since that time, the landscape has changed considerably, however. In fact, there are several other flap surgeries that can be performed using thigh tissue which result in a what Dr. LoTempio calls a “mini thigh lift.” But maybe you don’t need a butt lift so much as you need proper underwear to flatter your butt shape.
Bunions

You love those high-heeled shoes, but your feet don’t. Now you have a bunion—a painful bony bump on the joint at the base of your toe which pushes one toe against another, sometimes even causing the toes to overlap, and inevitably causing considerable pain. Bunions are also unsightly, but that’s beside the point when it comes to insurance coverage. According to Josef J. Geldwort, MD, DPM, a sports medicine doctor and podiatrist in New York, “more health insurance companies will cover a bunion procedure than you may think. It all depends on the circumstances present.” If you have bunions and assumed your insurance wouldn’t cover their removal, you might be pleasantly surprised to find that many insurance companies provide coverage when bunions are associated with pain and functional limitations. The insurance company, Cigna, addresses the medical aspects of bunion surgery here. Here are some ways to deal with your bunion pain without surgery.
Varicose veins

“I’ve had many patients tell me that they were reluctant to see a doctor for their varicose veins because they thought varicose veins were a cosmetic problem, so their health insurance plan wouldn’t pay for treatment,” says Steven D. Cox, MD, an Ohio-based surgeon. It is true that most health plans won’t pay for treatment of spider veins, but they will authorize treatment of varicose veins if we can demonstrate medical necessity. “If you have large, bulging veins on your legs or thighs, you probably have a problem called venous insufficiency, which meets the criteria for medical necessity for insurance plans,” he says. According to Dr. Johnson, the rule is that “generally, if your varicose veins present with painful symptoms and you’ve tried and failed with non-invasive therapies such as support stockings and sclerosing therapy, then insurance will cover the surgery.” It probably won’t alleviate the need for surgery, but horse chestnuts may provide some relief for the discomfort of varicose veins.
Content continues below ad





